Abstract
Early autologous hematopoietic stem cell transplantation (auto-HCT) is recommended for transplant-eligible patients (pts) with newly diagnosed multiple myeloma (MM). However, gastrointestinal toxicities, i.e., oral mucositis (OM), nausea and diarrhea, are the major limitation to the use of auto-HCT especially in the elderly population which constitute a significant proportion of MM pts, where the median age at diagnosis is 68 years. There is an unmet need for measures to minimize non-hematological toxicities without compromising melphalan anti-myeloma efficacy; this could lead to expansion of transplant eligibility to older pts. Amifostine, a FDA-approved cytoprotective agent to prevent OM for Head and Neck cancer, may reduce HDM-associated GI toxicity. We conducted a case-control study comparing auto-HCT with or without amifostine for MM pts.
Methods
pre-transplant amifostine has been incorporated to standard protocol for all MM patients underwent auto-HCT at University Hospitals Cleveland Medical Center (UH) for the last decade. One hundred and seven pts treated at UH who received amifostine, from January 2007 to July 2014, were compared to 114 matched-control pts treated at MD Anderson Cancer Center (MDACC) without use of this agent. The institutional review boards at both institutions approved the study. Amifostine 740 mg/m2 was administered as a bolus infusion at 24 hours and 15 minutes before HDM. All pts received ice chips peri-melphalan infusion. Survival outcomes were measured from the date of auto-HCT to the date of disease relapse or progression, Survival distribution was estimated using Kaplan-Meier methods. The effect of treatment on OS and PFS was estimated using a Cox model after controlling for the effects of age, gender, and number of prior therapies, time from diagnosis to transplant, Eastern Cooperative Oncology Group (ECOG) performance status and number of infused CD34+ cells.
Results
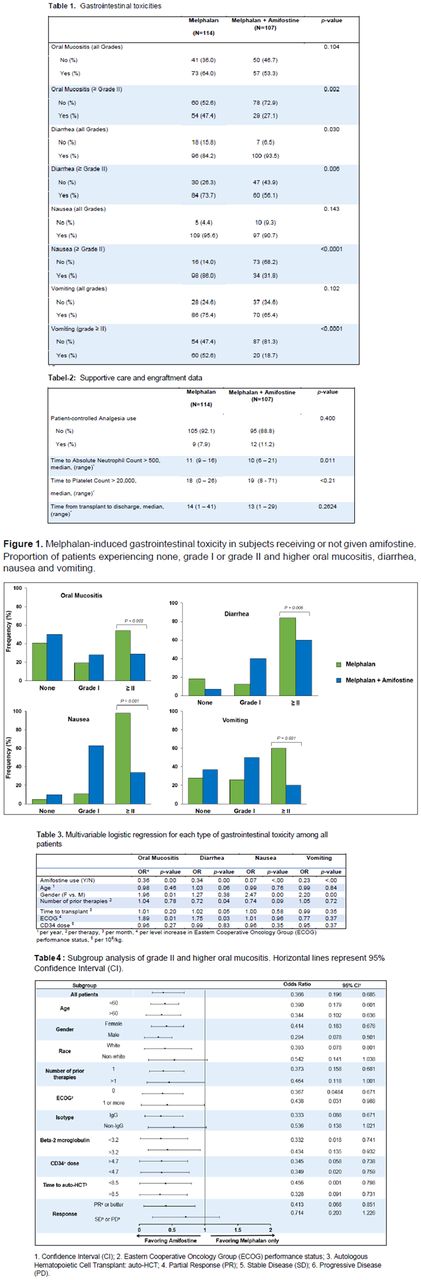
Pts' characteristics were similar in both groups.Median follow-up of surviving pts was 35 (range 2-100) months in both cohorts. Amifostine therapy was well tolerated without any serious adverse effects. There was no significant difference between all-grade OM, nausea or vomiting between the two cohorts. However, > grade II GI toxicities were significantly lower in the amifostine group as follows: OM: 27.1% vs 47.4% (P=0.002), diarrhea: 56.1% vs. 72.7% (P=0.006), nausea: 31.8% vs. 86.0% (P=0.0001) and vomiting: 18.7% vs. 52.6%, (P=0.0001) (Figure-1) (Table-1). Median time to platelet engraftment was similar between the two groups while neutrophil engraftment period was shorter with use of amifostine (10 vs. 11 days, P=0.011) (Table-2). Multivariable logistic regression showed that use of amifostine pre-transplant was associated with a significant decrease in OM, diarrhea, nausea and vomiting. Pts who received amifostine and melphalan developed grade ≥ II OM significantly less often than those given melphalan alone with odds ratio (OR) = 0.366 (95% CI: 0.196-0.685, P=0.001; Table 3). Female gender was associated with a significant increase in OM, nausea and vomiting. Female pts were more likely to develop grade ≥ II OM with OR of 1.967 (P=0.017). Similarly, an ECOG performance status (PS) of ≥ 2 was associated with a significant increase in OM and diarrhea. For every additional score of ECOG, the risk of having grade ≥ II OM increased 1.89 fold (p=0.015). Subgroup analysis of grade II and higher OM rates are shown in Table-4. Use of amifostine was associated with reduced grade II or higher GI toxicity after adjusting for the effects of age, gender, number of prior therapies, time from diagnosis to transplant, ECOG PS and infused CD34 cell dose. There was no detrimental effect of amifostine on progression-free or overall survival.
Conclusions
Our analysis indicates that the use of two amifostine doses of 740 mg/m2 before auto-HCT is safe and associated with significant reduction in grade II and higher GI toxicities without any deleterious effect on engraftment or anti-myeloma efficacy. Amifostine use could conceivably allow further melphalan dose-intensification for pts with resistant or high-risk disease. Also, pre-treatment with amifostine potentially could expand the utilization of auto-HCT for modestly frail MM pts that might not be considered eligible for this treatment modality. The protective effect of amifostine should be confirmed in randomized trial.
Malek: Celgene: Speakers Bureau; Takeda: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sanofi: Membership on an entity's Board of Directors or advisory committees. Cooper: Novartis: Research Funding. Caimi: Abbvie: Equity Ownership; Incyte: Equity Ownership; Celgene: Speakers Bureau; Seattle Genetics: Equity Ownership. De Lima: Pfizer: Membership on an entity's Board of Directors or advisory committees; Celgene Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal